| Can shoulder dystocia be resolved without fetal injury when it does occur? The management of shoulder dystocia
The preponderance of evidence from the literature on shoulder dystocia shows clearly that:
(1) Shoulder dystocia cannot be predicted with any degree of accuracy and
(2) Shoulder dystocia cannot be prevented by any specific strategies or maneuvers.
The question thus arises "How should shoulder dystocia be managed when it does occur? Can it be resolved successfully without injuring the baby or the mother?"
Much has been written on this subject. Multiple maneuvers claiming to be able to resolve shoulder dystocia have been described. We will now take a look at what these maneuvers are, how they are performed, and how effective they have proven to be.
Recognition
The first step in treating shoulder dystocia is recognizing when it occurs.
There are two main signs that a shoulder dystocia is present:
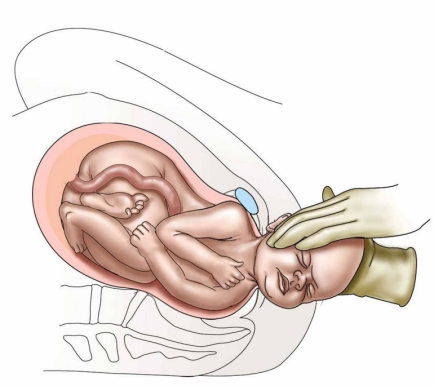
(1) The baby's body does not emerge with standard traction and maternal pushing after delivery of the fetal head.
(2) The "turtle sign". This is when the fetal head suddenly retracts back against the mother's perineum after it has emerged from the vagina. The baby's cheeks bulge out, resembling a turtle pulling its head back into its shell. This retraction of the fetal head is caused by the baby's anterior shoulder being caught on the back of the maternal pubic bone, preventing delivery of the remainder of the baby.
Turtle Sign

photo by Kristina Kruzan, kristinakruzan@gmail.com
Traction: "Excessive" or "Necessary" Force?
Babies rarely fall out of the pelvis -- nor should they. Especially in an age where conduction anesthesia (epidurals, spinals) is used routinely, often a mother must push several times in order to deliver the remainder of her baby after its head is born. To facilitate the passage of the baby's anterior shoulder under mother's pubic bone, it is standard practice for the deliverer to deflect the baby's head downwards. It is of interest that plaintiff lawyers in shoulder dystocia medical-legal cases and the expert witnesses they hire often say that there should be no downward traction utilized in resolving a shoulder dystocia delivery. Yet as the 2014 ACOG treatise on neonatal brachial plexus palsy states,
Because the position of the infant within the maternal pelvis will be at some angle relative to the horizontal plane (e.g., delivery table) during the final cardinal movements of labor, axial traction is generally applied in the direction or vector below the horizontal plane (also referred to as downward axial traction as distinguished from downward lateral traction or lateral bending).
It is also often said in court rooms that traction should never be applied to the fetal head during attempts to resolve a shoulder dystocia. This is certainly not the case. Unless a baby falls out of a mother—which is certainly not what happens with a shoulder dystocia—some traction—“gentle”, “moderate”—is always applied by the delivering clinician to the infant’s head. This is, in fact, the standard of care practiced by obstetricians across the United States and is the procedure describe in multiple obstetrical textbooks (see, for instance the Williams Obstetrics textbook or the Stanford Handbook of Obstetrics. Such assisting of delivery of the head is a necessary and approved obstetrical practice.
Normal
Delivery Traction
What about the slippery term "excessive force"? This term conveys an image of an obstetrician pulling with all his or her might, propping a leg against a delivery table for support, etc.
Students of shoulder dystocia have long sought to determine exactly what degree of force constitutes "excessive force". Some investigators, such as Allen (1991) and Gonik, have even tried to determine this by using specially-constructed gloves with piezoelectric fingertip sensors to measure pressures at delivery.
It would seem on the face of it that the use of strong force to attempt to deliver an impacted shoulder should be universally condemned. But one must take into account the circumstances involved. There are times when all maneuvers have been attempted to resolve a shoulder dystocia and when the only options left are either a maximal effort to extract the baby, including greater than desired forces, hypoxic neurologic damage, or fetal death. In such cases, faced with the ultimate catastrophe of the death of a baby, the risk of brachial plexus or other fetal injury must be accepted.
What the physician must not do when a shoulder dystocia occurs is to lose composure. Most shoulder dystocias occur unexpectedly. But by restraining panic, keeping a cool head, and employing a previously thought-out—and trained for--set of maneuvers, almost all shoulder dystocias can be resolved with excellent results for both baby and mother. The term "almost all" is used advisedly as sometimes, even in the most expert hands, and even with relatively mild shoulder dystocias, fetal or maternal injury will occur.
What to do when a shoulder dystocia occurs
Several things should be done as soon as a shoulder dystocia is recognized. First, the obstetrician should announce that a shoulder dystocia is present. He or she should then request that a second obstetrician called, if possible, and should ask the nurses to make sure that extra personnel are available. The obstetrician should also stay informed of the time that has elapsed since delivery of the head. One means of doing this is to designate someone to call out the time since delivery of the head at fixed intervals -- perhaps every 30 seconds. Pediatric or neonatal assistance should also be called so as to be available to evaluate and potentially resuscitate the baby after delivery. Anesthesia staff should be summoned. If sufficient staff is available, one person should be designated as a note taker to record the timing of events.
How much time does one have to resolve a shoulder dystocia before hypoxic brain injury becomes a significant risk?
In general, the operator has up to five minutes to deliver a previously well-oxygenated term infant before an increased risk of asphyxial injury occurs.
Several studies over the years have attempted to determine the drop in fetal pH in the minutes following the onset of a shoulder dystocia. As noted previously, Wood (1973) was the first to examine this question in detail. He determined that for each minute during the interval between delivery of the fetal head and trunk in a shoulder dystocia delivery a fetus’s pH drops 0.04 units per minute. Subsequent studies have challenged this data; Leung in 2011 found the rate of pH drop per minute during a shoulder dystocia to be 0.01 unit. Yet as Gherman has shown (2006), there is not a good correlation between the head-to-body delivery interval and pH, pCO2, and pO2.
More recently, both Leung (2011) and Lerner (2011) have shown that the delivering clinician has roughly 4-5 minutes to resolve a shoulder dystocia before the risk of ischemic neuropathy becomes significant. This time frame of course depends upon the oxygenation and acidosis status of the fetus prior to the onset of the shoulder dystocia.
The Maneuvers
Once a shoulder dystocia is recognized, there are several specific obstetrical maneuvers that have been proven to be of benefit in assisting in the resolution of the dystocia.
(For an excellent in-depth review of shoulder dystocia resolution maneuvers and the traction forces involves, see Stitely and Gherman [2014].)
McRoberts maneuver and suprapubic pressure
The first two maneuvers generally attempted in order to resolve a shoulder dystocia are (1) McRoberts maneuver and (2) suprapubic pressure. In fact both of these maneuvers are so benign and so effective that they are sometimes employed prophylactically in anticipation of a potential shoulder dystocia.
click on
image to view larger image
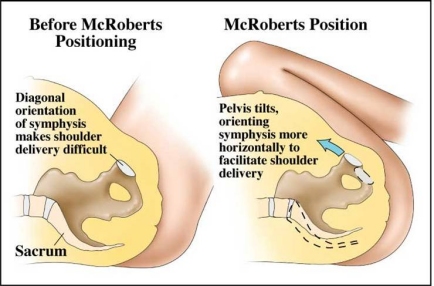
McRoberts maneuver is named for William A. McRoberts, Jr. who popularized its use at the University of Texas at Houston. It involves sharply flexing the legs upon the maternal abdomen. By doing this, the symphysis pubis is rotated cephalad and the sacrum is straightened. In a high percentage of cases this by itself suffices to free the impacted anterior shoulder.
Suprapubic pressure is the attempt to manually dislodge the anterior shoulder from behind the symphysis pubis during a shoulder dystocia. It is performed by an attendant making a fist, placing it just above the maternal pubic bone, and pushing the fetal shoulder in one direction or the other. Since shoulder dystocias are frequently caused by an infant's shoulders entering the pelvis in a direct anterior-posterior orientation instead of the more physiologic oblique diameter, pushing the baby's anterior shoulder to one side or the other from above can often change its position to the oblique which will allow its delivery. Suprapubic pressure in conjunction with McRoberts maneuver is often all that is needed to resolve 50-60% of shoulder dystocias.
In order to show more clearly how McRoberts maneuver aids in the resolution of a shoulder dystocia, Gherman (2000) performed a study in which he took x-rays of 36 women in the dorsal lithotomy position before and after McRoberts positioning. He found that there were no significant changes in the anterior-posterior and transverse diameters of the pelvic inlet, midpelvis, and pelvic outlet. There also was no increase in the obstetric, the true, and the diagonal conjugates of the pelvis. Thus, McRoberts maneuver does not change the actual dimensions of the maternal pelvis. What it does do, however, is to rotate the symphysis pubis toward the maternal head. This significantly changes the angle of inclination between the top of the symphysis and the top of the sacral promontory. This, in conjunction with the flattening of the sacrum, is often enough to allow stuck fetal shoulders to deliver.
Suprapubic
Pressure

A study by Gonik and Allen (1989) confirmed that this is the case. They showed that implementation of McRoberts maneuver can significantly reduce required fetal extractive forces and brachial plexus stretching in shoulder dystocias. In addition to allowing the anterior shoulder to slide more freely under the bottom of the symphysis, the flattening of the sacrum relative to the lumbar spine allows the posterior fetal shoulder to more easily pass over the sacrum and through the pelvic inlet.
How successful is McRoberts maneuver? Gherman (1997) observed 250 shoulder dystocia deliveries at USC from 1991 to 1994 and reported that McRoberts maneuver alone was successful in resolving 42% of them. Fifty-four percent of all shoulder dystocias were resolved by a combination of McRoberts maneuver, suprapubic pressure and/or procto-episiotomy without further maneuvers being necessary. McFarland (1996) reported similar findings: 39.5% of shoulder dystocias resolved with McRoberts maneuver alone while 58% resolved with a combination of McRoberts maneuver and suprapubic pressure.
Although McRoberts maneuver and suprapubic pressure are generally safe, it is possible to cause maternal injury by performing them. Symphyseal separations and transient femoral neuropathies from overly aggressive hyperflexing of the maternal thighs have been reported. Whether or not an infant might be subject to injury with these maneuvers has been questioned by Gurewitsch and Allen (2005)--see below.
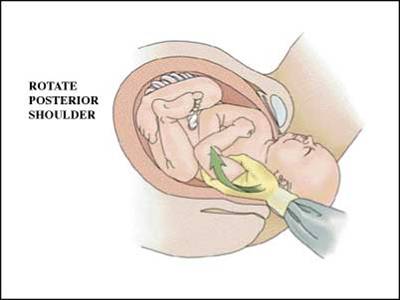
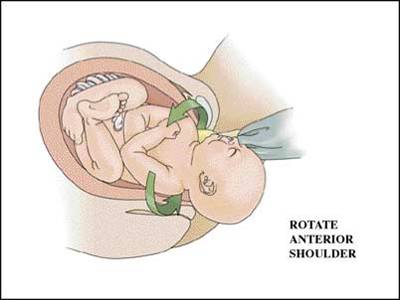
Wood's Screw maneuver
First described in the literature in 1943, this procedure involves the progressive rotation of the posterior shoulder in corkscrew fashion to release the opposite impacted anterior shoulder. In its classic description, pressure is applied on the posterior shoulder's anterior surface. A variation of this -- the Rubin's maneuver -- involves pushing on the posterior surface of the posterior shoulder. In addition to the corkscrew effect, pressure on the posterior shoulder has the advantage of flexing the shoulders across the chest. This decreases the distance between the shoulders, thus decreasing the dimension that must fit through the pelvis. Gurewitsch and Allen (2005) feel that these maneuvers place less stretch on a fetus’s brachial plexus than do the McRoberts maneuver or suprapubic pressure.
Delivery of the posterior arm
Another effective maneuver for resolving shoulder dystocias is the delivery of the posterior arm. In this maneuver, the obstetrician places his or her hand behind the posterior shoulder of the fetus and locates the arm. This arm is then swept across the fetal chest and delivered. With the posterior arm and shoulder now delivered, it is relatively easy to rotate the baby, dislodge the anterior shoulder, and complete delivery of the remainder of the baby.
The major risk of this procedure is that of fracturing the humerus. Gherman (1998) reported 11 (12.4%) humeral fractures in 89 shoulder dystocias resolved by delivery of the posterior arm. However, since almost all humeral fractures heal quickly and without permanent damage, this would appear to be a small price to pay for the successful delivery of an infant in a life threatening situation.
Delivery of the posterior shoulder: Menticoglou and the posterior axillary sling
Menticoglou (2006) first described putting a finger into posterior axilla of the fetus to pull the posterior shoulder downward. This enables the grasping of the posterior arm, allowing it to be delivered, followed by delivery of the trunk. In 2009 Hofmeyr reported on a variation of this procedure. Instead of just using a finger, Hofmeyr recommends placing a soft plastic catheter sling around the posterior axilla and using that for traction.
Many, however, have voiced skepticism about these maneuvers. For if one has enough access to the fetal shoulder and axilla to place a finger or a sling around them, one wonders why the delivery could not have been performed as a routine rotational maneuver. Moreover, Cluver in 2015 reported on the use of the axillary sling in 19 cases. In five the baby had already died. Delivery was successful in 18 cases. There were 3 posterior humerus fractures, four cases of transient Erb palsy, and one case of permanent Erb palsy.
There have been multiple other techniques and procedures described over the years to resolve shoulder dystocias. None of these, however, have reached the level of "mainstream". Some of these are the Zavanelli maneuver, deliberate fracture of the clavicle, symphysiotomy, the "all-fours" maneuver, and fundal pressure.
Zavanelli maneuver
Although almost certainly performed by obstetricians and midwives in the past, this maneuver was first described in the obstetrical literature by Dr. Zavanelli, an obstetrician in private practice in Pleasanton, California in 1977. Dr. Zavanelli reported that during one difficult shoulder dystocia delivery, after having attempted all other maneuvers, he finally resorted to flexing the fetal head and pushing it back up into the vagina. He was then able to perform an emergency cesarean section and deliver a live baby.
The first step in any cephalic replacement maneuver (now called the Zavanelli maneuver) is to set up for an emergency cesarean section. The fetal head is rotated to the occiput anterior position and flexed. Constant firm pressure is applied while pushing the head back into the vagina. Tocolytic agents such as terbutaline, nitroglycerin, or uterine-relaxing general anesthesia may be administered to facilitate this process. Cesarean section must be performed immediately after replacement of the head.
The Zavanelli maneuver enjoys a mixed reputation. O'Leary (1993) reported on 59 women who had undergone replacement of the fetal head following unsuccessful attempts at vaginal delivery. All but 6 of these infants were successfully replaced and delivered by Cesarean section. He therefore suggested that the Zavanelli maneuver might not need to be used as a last resort maneuver but might be considered if any undue difficulty were encountered with a shoulder dystocia.
But a closer look at the data O’Leary reports is less than reassuring. In his series, the delay of cephalic replacement following delivery of the head ranged from 5 minutes to greater than 30 minutes. He was unable to replace the fetal head in six instances and he reported replacement as "difficult" in five. Apgar scores at 5 minutes were less than 6 in 61% of these babies and were less than 3 in 27%. Four babies in his series had seizures in the nursery, two had permanent neurologic injury, five experienced a permanent Erb palsy, and two died. Three percent of the mothers experienced a ruptured uterus and 5% suffered uterine lacerations.
Although Sanberg (1999) reported a much more optimistic experience with the Zavanelli maneuver -- 77.3% “success rate” involving 84 cases, neonatal complications in his series included clavicular fractures, humoral fractures, Erb palsies, quadriplegia, brain damage, mental retardation, various degrees of cerebral palsy and even mortality.
The data from these two series is sobering. While it is incumbent upon all obstetricians to know about the Zavanelli maneuver and to be able to perform it when other options for shoulder dystocia resolution have been exhausted, its significant potential for fetal and maternal injury must relegate it to the status of a "last ditch" procedure.
Transabdominal shoulder rotation (“Abdominal rescue”)
O’Shaughnessy in 1998 described another “last ditch” approach. He reported two cases in which, after unsuccessfully performing multiple shoulder dystocia resolution maneuvers, he performed a laparotomy and hysterotomy and then manually rotated the fetus’s stuck shoulders until he was able to complete a vaginal delivery.
Deliberate fracture of the clavicle
Almost all detailed accounts of shoulder dystocia include “deliberate fracture of the clavicle” as one modality for resolving this situation--but there are few accounts of this procedure actually being performed. In practice, the clavicle poses a formidable obstacle to its fracture. It is a significant bone, even in a fetus. Although the fracture of the clavicle certainly would decrease the transverse diameter of the chest and shoulders, the potential of damaging the great vessels, fetal lungs, and other structures make this an extremely hazardous procedure even if it were possible to perform easily. In fact most descriptions of transection of the clavicle involve fetuses that are already dead and require the use of a large scissors or other sharp instrument for cutting the bone.
Symphysiotomy
Symphysiotomy is a procedure that had been performed in desperate situations in the past and is now performed only in areas remote from the ability to perform Cesarean sections on a rapid basis. The theory is that by transecting the firm ligaments joining the left and right symphyseal bones, an additional 2-3cm in pelvic circumference can be gained. In most cases this will allow the anterior shoulder of a stuck fetus to be delivered beneath the symphysis. The benefit of the procedure is that it can be performed rapidly -- it usually takes 5 minutes or less -- and can be done under local analgesia. In subsequent pregnancies a woman who has undergone a symphysiotomy has an intact uterus and a slightly enlarged pelvis.
The symphyseal separation obtained by symphysiotomy affects the transverse diameters of the pelvis, particularly those of the mid cavity and outlet. The area of the pelvic brim increases by 8% for every 1cm of joint separation.
The technique involves abducting the thighs to 80 degrees (but no further). A 2cm skin incision is made over the mons. With an index finger in the vagina displacing the urethra, the scalpel is inserted in the midline of the mons at the junction of the upper and middle thirds of the symphysis. If difficulty is experienced finding the ligament, a needle can be placed first. The blade is inserted until it impinges on the vaginal epithelium as determined by the finger in the vagina. Using the upper symphysis as a fulcrum, the knife is rotated, cutting the lower 2/3rds of the symphysis. The knife is then turned 180 degrees and the upper third of the symphyseal ligament is transected. Separation thus obtained is between 2 and 3cm -- the width of a thumb.
Following symphyseal separation, the bladder must be drained for five days. The patient is kept in bed on her side for three days. Sometimes the knees are tied together to enforce this position. On the fourth day the patient may sit in bed and on the fifth day walk. Results in terms of maternal recovery are uniformly excellent with return of full ambulation and pelvic stability.
The major risk is to maternal soft tissues including the bladder and urethra. As with many techniques, the more experience one obtains with procedure, the more quickly it can be performed and the lower the complication rate. Hartfield published a detailed description of symphysiotomy in 1973 in order to remind obstetricians that such a procedure exists. Although not advocating it in developed countries as a first step, he does state that it can be effected very quickly and may in some instances save a fetus' life when all other measures to resolve a shoulder dystocia have been exhausted. As he says in a second article he published on the subject in 1986,
The risk of maternal soft tissue trauma has to be weighed against the almost certain loss of the baby if other methods of vaginal delivery are proving unsuccessful.
All-fours maneuver
In 1976, Ina May Gaskin, a midwife, described a maneuver for the resolution of shoulder dystocia that involves placing the gravid mother on her hands and knees. Bruner (1998) used this procedure in 82 deliveries complicated by shoulder dystocia and was able to resolve the dystocia in 68 cases (82%) with this maneuver alone. The average time needed to move the mother into this position and to complete delivery was reported to be 2-3 minutes. Unfortunately, there was no detailed description of fetal and maternal outcome in this report. Also, reports about this procedure have generally been in the midwifery literature, involving a patient population less likely to have epidural anesthesia and thus more likely to be fully mobile.
It may be that the "all-fours maneuver" is merely another means of changing the angle of the symphysis in relation to the stuck shoulder, akin to McRoberts maneuver. Since the all-fours maneuver involves a gravid woman at the end of her pregnancy, exhausted by a long labor, often with an epidural in place, being moved quickly out of her delivery position onto all fours on her bed or on the floor, the practicality of this maneuver for a general obstetrical population is open to question. Unless more data is presented as to its efficacy and utility, it cannot be considered a standard procedure for the resolution of shoulder dystocia.
Are any particular maneuvers better than the shoulder dystocia resolution maneuvers?
This is not at all clear. There have been multiple reports by different authors claiming various degrees of success with each of the shoulder dystocia resolution maneuvers.
Leung in 2011 evaluated delivery methods in 205 cases of shoulder dystocia. He found that following the failure of McRoberts maneuver the subsequent application of rotational methods or of posterior arm delivery has similarly high rates of success although the former may be associated with less fetal injury. The rate of either brachial plexus injury or humoral fracture with rotational methods was 4.4% vs. 21% with delivery of the posterior arm. Leung et al suggest that delivery of the posterior arm is less safe than rotational methods.
Also, Leung’s success rate with McRobert’s maneuver alone in his largely Chinese patient population was only 25% as compared to multiple American studies showing the success rate with this maneuver to be in the 40% range.
On the other hand, Hoffman (2011) reviewed 132,098 deliveries in which there were 2018 shoulder dystocias for a rate of 1.5%. One hundred one of these--5.2%--resulted in a neonatal injury. Delivery of the posterior shoulder was associated with the highest rate of successful delivery compared to all other maneuvers with no difference in the rates of damage to the newborn. Hoffman recommends that the clinician move to delivery of the posterior shoulder if McRoberts maneuver and suprapubic pressure prove unsuccessful in the management of shoulder dystocia. The need for additional maneuvers was associated with higher rates of neonatal injury.
Finally, Spain (2015), in a study of 231 women who experienced a shoulder dystocia,
found that individual maneuvers were not associated with composite morbidity, neonatal injury, or neonatal depression after adjusting for parity and duration of shoulder dystocia. His conclusion:
There was no association between shoulder dystocia maneuvers and neonatal morbidity after adjusting for duration, a surrogate for severity. Our results demonstrate that the clinician should utilize the maneuver most likely to result in successful delivery.
So what can be said about the efficacy of the various shoulder dystocia resolution maneuvers?
1. The various maneuvers have not been subjected to a randomized trial
2. No maneuver has been clearly shown to be superior to any other in terms of successfully resolving a shoulder dystocia or reducing the rate of newborn injury.
What are some of the recommended protocols for resolving shoulder dystocia?
Many authors have proposed various protocols of prescribed maneuvers for the resolution of shoulder dystocia. Most are similar with only minor variations.
When a shoulder dystocia is recognized, it is generally agreed that McRoberts maneuver and suprapubic pressure should be implemented rapidly and simultaneously. These by themselves will resolve more than half of all shoulder dystocias. If the shoulder dystocia persists, other maneuvers can be performed in any order. These include the Wood's screw or Rubins maneuver in either the clockwise or counter clockwise direction, attempting to deliver the posterior arm, and, in extremis, consideration of such techniques as the Zavanelli maneuver or symphysiotomy.
ACOG, in its bulletin on shoulder dystocia (2002, reaffirmed 2015), proposed the following sequence of maneuvers for reducing a shoulder dystocia:
1) McRobert’s maneuver and suprapubic pressure
2) Episiotomy—controversial
3) Rotational maneuvers
4) Delivery of posterior arm
Harris in a 1984 paper recommended a similar protocol:
1) McRoberts maneuver.
2) Suprapubic pressure.
3) Large mediolateral episiotomy if above steps fail.
4) Wood's screw maneuver.
5) Attempt to free posterior arm.
Gherman (1998) discussed the protocol for managing shoulder dystocia utilized at that time at the University of Southern California:
McRoberts maneuver
Suprapubic pressure
Procto-episiotomy
Wood's corkscrew maneuver
Posterior arm extraction.
Zavanelli maneuver or symphysiotomy if all else fails.
McFarland (1996) reported that the use of two maneuvers alone --McRoberts and suprapubic pressure -- resulted in the resolution of 58% of 276 cases of shoulder dystocia in his series. He found that the addition of the Wood's Screw maneuver and delivery of the posterior arm were sufficient to resolve the shoulder dystocia in all remaining cases. He also found that there was a direct correlation between the rate of brachial plexus injury and the number of maneuvers employed to resolve the shoulder dystocia. A second correlation he found was that as the fetal weight increased, the number of maneuvers required to resolve shoulder dystocias increased.
Sentilhes (2016) discussed the guidelines for shoulder dystocia resolution from the French College of Gynecologists and Obstetricians (CNGOF)
Ask for help.
Perform McRoberts maneuver with or without suprapubic pressure.
Apply traction along the umbilical-coccygeal axis
Do either reverse Woods corkscrew maneuver or deliver posterior arm
Perform an episiotomy if one has not yet been performed one
Repeat maneuvers
Go to third line maneuvers.
Sentilhes adds two notes:
1. The available data do not allow us to conclude that any one of these maneuvers is superior to any other.
2. The performance of these obstetrical maneuvers for treating shoulder dystocia does not routinely require an episiotomy.
As has been shown, different authors recommend different combinations of maneuvers in attempting to resolve shoulder dystocias. But what every author emphasizes, and what the ACOG bulletin stresses, is that the most important aspect of resolving a shoulder dystocia is for the obstetrician to have a clear-cut, well thought-out sequence of maneuvers already in mind when a shoulder dystocia is encountered. The general consensus is that the best results in resolving shoulder dystocias are obtained when an obstetrician:
(1) Recognizes the shoulder dystocia
(2) Knows the different maneuvers involved in attempting to resolve shoulder dystocia
(3) Implements them in a carefully controlled, calm, and organized fashion.
next >>
Copyright © 2017 Henry Lerner |