Following shoulder dystocia deliveries, 20% of babies will suffer some sort of injury, either temporary or permanent. The most common of these injuries are damage to the brachial plexus nerves, fractured clavicles, fractured humeri, contusions and lacerations, and birth asphyxia.
Brachial plexus injury
Brachial plexus injury is the classic injury following shoulder dystocia. It was first described by Duchenne in 1872.
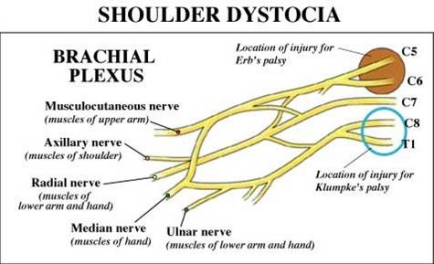
The brachial plexus consists of the nerve roots of spinal cord segments C5, C6, C7, C8, and T1. (See accompanying diagram). These nerve roots form three trunks which divide into anterior and posterior divisions. The upper trunk is made up of nerves from C5 and C6, the middle trunk from undivided fibers of C7, and the lowermost trunk is made up of nerves from C8 and T1.
click on
image to view larger image

There are two major types of brachial plexus injury: Erb palsy and Klumpke palsy.
Erb palsy, the more commonly occurring form, involves injury to the upper trunk of the brachial plexus (nerve roots C5 through C7). This palsy affects the muscles of the upper arm and causes abnormal positioning of the scapula: "winging". The supinator and extensor muscles of the wrist that are controlled by C6 may also be affected. Sensory deficits are usually limited to the distribution of the musculo-cutaneous nerve. Together, these injuries result in a child having a humerus that is pulled in towards the body (adducted) and internally rotated with the forearm extended. Some have described this as the "waiters tip" position.
Klumpke palsy involves lower trunk lesions from nerve roots C7, C8, and T1. In this injury the elbow becomes flexed and the forearm supinated (opened up, palm-upwards) with a characteristic clawlike deformity of the hand. Sensation in the palm of the hand is diminished.
click on
image to view larger image
Patients seen with upper lesions immediately after birth—Erb palsy—have a better prognosis than those with lower brachial plexus injuries—Klumpke palsy. Whereas upwards of 90 to 95% of all Erb palsies totally resolve, only 60% of Klumpke palsies do. Interestingly, those brachial plexus injuries associated with non-shoulder dystocia deliveries persist more often than those occurring following deliveries in which a shoulder dystocia was documented.
Brachial plexus injuries can also produce secondary effects. Muscle imbalances in the hand, arm, and shoulder caused by brachial plexus injuries may result in osseous deformities of the shoulder and elbow and in dislocations of the radial head. The development of the affected arm may be compromised resulting in its being as much as 10 cm shorter than the nonaffected arm.
While a sense of the degree and type of injury can be estimated by physical exam and clinical observation of the baby’s movement limitations, the true extent of brachial plexus injuries and the specific pathophysiology involved can only be definitively determined during surgical exploration of the brachial plexus at the time of a reparative procedure.
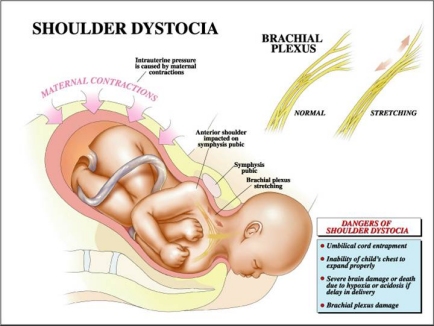
It has been traditionally thought that most brachial plexus injuries result from stretching of the nerves of the brachial plexus during delivery. While this likely accounts for many brachial plexus injuries, reports of such injuries following deliveries in which there was no shoulder dystocia (Allen 2005, Lerner 2008, Ouzounian 2012) has led investigators to question whether or not brachial plexus injuries might have other etiologies. Such etiologies might be the stretching of the brachial plexus that can occur by the forces of labor (uterine contractions and maternal pushing) and—less likely—intrauterine cerebrovascular accidents (strokes), overstretching of the brachial plexus from fetal movement during the pregnancy, or spontaneous mal-development of the brachial plexus.
In some brachial plexus injuries sympathetic nerve fibers that traverse T1 can be damaged. This can result in depression of the eyelid and drooping of the mouth on the affected side, a constellation of symptoms called Horner's Syndrome.
click on
image to view larger image
The natural history of brachial plexus injury
Fortunately, most brachial plexus birth injuries are transient. The majority of such injuries resolve by three months, with a range of 2 weeks to 12 months. Only 4 to 15% result in some degree of permanent injury as reported by various authors in the list below:
Johnson (1979) 7.8%
Sandmire (1988) 11.8%
Nocon (1995) 4%
Eckert (1997) 5-22%
Graham (1997) 20%
Chauhan (2014) 8%
Average: ~10%
Even though shoulder dystocia occurs in only 0.5% to 1.5% of all deliveries, the fact that there are approximately 3 million vaginal deliveries a year in United States means that many hundreds of babies will experience permanent brachial plexus injury. A little math tells the story:
—If the rate of occurrence of shoulder dystocia is approximately 0.5 to 1.5%, and
—If the rate of brachial plexus injury is 10% in these deliveries, and
—If the rate of permanent injury is 10% of all brachial plexus injuries, then the rate of permanent brachial plexus injury will be one in 6,666-20,000 vaginal deliveries
This means that there will be approximately 150-450 babies born each year in the United States with permanent brachial plexus injuries. In addition, there will be babies who will suffer severe central neurologic injury such as cerebral palsy from asphyxia. There will even be babies who will die following severe shoulder dystocias. It is for these reasons that shoulder dystocia injuries have become an important area of medical — and medical-legal — concern.
Treatment options and prognosis
As mentioned, the majority of brachial plexus injuries will resolve spontaneously over the course of several months to a year. Physical therapy is usually employed within weeks of birth to help strengthen muscles whose nerve supply has been damaged. For those injuries that are permanent there are two modes of therapy.
First, physical therapy can strengthen muscles that are only partially denervated, strengthen surrounding muscles to compensate for functional loss and improving the range of motion of the affected shoulder, arm, elbow, or hand.
Second, surgical therapy in the form of nerve grafting or muscle transposition may be undertaken. There is, however, great controversy about the efficacy of such surgical procedures in improving the outcome of those with brachial plexus injuries. Several orthopedic and neurosurgeons from around the country who do this sort of surgery frequently report various degrees of improvement in many of their patients. Others in the field, however, refute these claims and feel that there is little or no benefit to such surgery.
�
Other neonatal injuries following shoulder dystocia deliveries
Fractured clavicle
The second most common injury suffered by infants following shoulder dystocia deliveries is a fractured clavicle. The incidence of this injury following shoulder dystocia is 10%.
If the fetal shoulders and chest are relatively large in relation to the maternal pelvis, significant pressure may be placed on them as they pass through the birth canal following delivery of the fetal head. In some infants, this pressure causes the clavicle to fracture. The overlapping of the ends of the broken clavicle reduces both the length between the shoulders and the diameter of the fetal chest and may allow the shoulders and chest to deliver. This "safety valve" effect may in fact help reduce the incidence of severe brachial plexus injuries.
The baseline clavicular fracture rate for all deliveries appears to be about 0.3%. Despite the fact that shoulder dystocia increases the risk of clavicular fracture 30 fold, approximately 75% of clavicular fractures are not associated with shoulder dystocia. Interestingly, although there are multiple reports of brachial plexus injuries following cesarean sections, clavicular fractures following cesarean sections are extremely rare.
Fractured humerus
This occurs in approximately 4% of infants with shoulder dystocia deliveries. While they may occur spontaneously, they are often the result of maneuvers employed to resolve a shoulder dystocia such as delivery of the posterior arm (see below). Such injuries heal rapidly and by themselves rarely result in litigation.
Contusions
The force with which an infant's shoulder is compressed against the maternal pubic bone and the pressure of the deliverer's hands on a fetus while performing various maneuvers to effect delivery will often result in bruises on the baby's body. Such bruising has often been cited by plaintiff attorneys as evidence that a baby has been handled roughly at delivery. In fact, such bruises are common even in routine deliveries not involving shoulder dystocia or fetal injury.
Fetal asphyxia
The most feared complication of shoulder dystocia is fetal asphyxia. It has been frequently demonstrated in both animal experiments and in retrospective analyses of babies born following dramatic cessation of umbilical blood flow (placental abruption, uterine rupture) that if babies are not delivered within five to 10 minutes they will suffer irreversible neurologic damage or death. Wood, in an often-quoted article from 1973, showed that in the time between delivery of the head and trunk of an infant, a baby’s umbilical artery pH declines at a rate of 0.04 units per minute. This would mean that at the five-minute mark following delivery of the fetal head, a baby's pH may have dropped from 7.2 — a common level after several hours of pushing — to 7.0, the level that defines asphyxia. By 10 minutes the pH would have dropped to 6.8.
Ouzounian (1998) reported that of 39 babies whose deliveries involved shoulder dystocia, 15 who suffered brain injury averaged a head-to-shoulder delivery interval of 10.6 minutes while the 24 babies also born following shoulder dystocia but without brain injury had a head-to-shoulder delivery interval of only 4.3 minutes.
Leung, in a more recent study—2011—found the drop in pH to be 0.011 per minute of head-to-body delivery interval as opposed to Wood’s 0.04/min. Both Leung (2011) and Lerner (2011) have shown that the risk of asphyxia during management of a shoulder dystocia delivery becomes significant at the 4-5 minute mark.
Cerebral palsy and fetal death are rare but unfortunately not unheard of consequences of prolonged head-to-shoulder delivery intervals following shoulder dystocia deliveries.
The reason for the increasing acidosis and asphyxia that occurs during a shoulder dystocia delivery is that once the fetal head emerges from the mother, the baby's umbilical cord becomes tightly compressed between its body and that of the mother's birth canal. This significantly decreases or totally cuts off blood flow between the mother and infant. If the pressure on the cord is not rapidly relieved, the consequences of lack of umbilical flow — decreased delivery of oxygen to the fetus — may occur.
Menticoglou (2016) has recently proposed a new explanation as to why resuscitation may fail in some neonates after shoulder dystocia deliveries: hypovolemic shock. He notes that not only oxygen is interrupted by compression of the umbilical cord during shoulder dystocias, but fluid and blood flow cease as well. The fetal heart can pump blood out through the thicker arterial walls of the umbilicus but the thinner venous walls may collapse, not allowing oxygenated blood to return to the fetus from the mother. If substantiated, this phenomenon may lead to a change in how babies are resuscitated after severe shoulder dystocias.
Some authors—for instance Westgate (2011)—feel that the differences in cord arterial pH seen among infants following shoulder dystocia deliveries more likely reflect the condition of a fetus in labor prior to the occurrence of a shoulder dystocia rather than the deterioration over time during the shoulder dystocia resolution process.
� Maternal injuries
The mother, too, is at some risk when a shoulder dystocia occurs. The most common complications she may suffer are excessive blood loss and vaginal and vulvar lacerations.
Significant maternal blood loss, which occurs in one quarter of all shoulder dystocia deliveries, may be seen either during the delivery or in the postpartum period. Its usual causes are uterine atony or lacerations of the maternal birth canal and surrounding structures. Such lacerations may involve the vaginal wall, cervix, extensions of episiotomies, or tears into the rectum. Uterine rupture has also been reported.
Because of the pressure directed upwards towards the bladder by the anterior shoulder when a shoulder dystocia occurs, post-partum bladder atony occurs frequently. Fortunately, it is almost always transient. Occasionally the mother's symphyseal joint becomes separated or the lateral femoral cutaneous nerve damaged, most likely the result of overaggressive hyperflexion of the maternal legs during attempts at resolving the shoulder dystocia.
next >>